Ready to launch your own podcast? Book a strategy call.
Frontlines.io | Where B2B Founders Talk GTM.
Strategic Communications Advisory For Visionary Founders
Conversation
Highlights
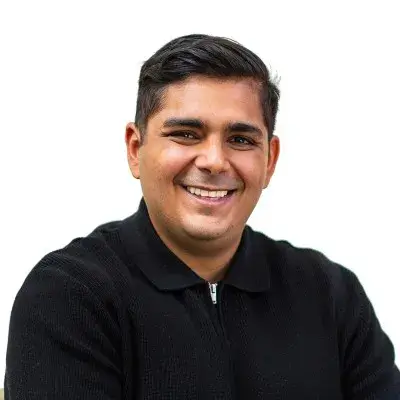
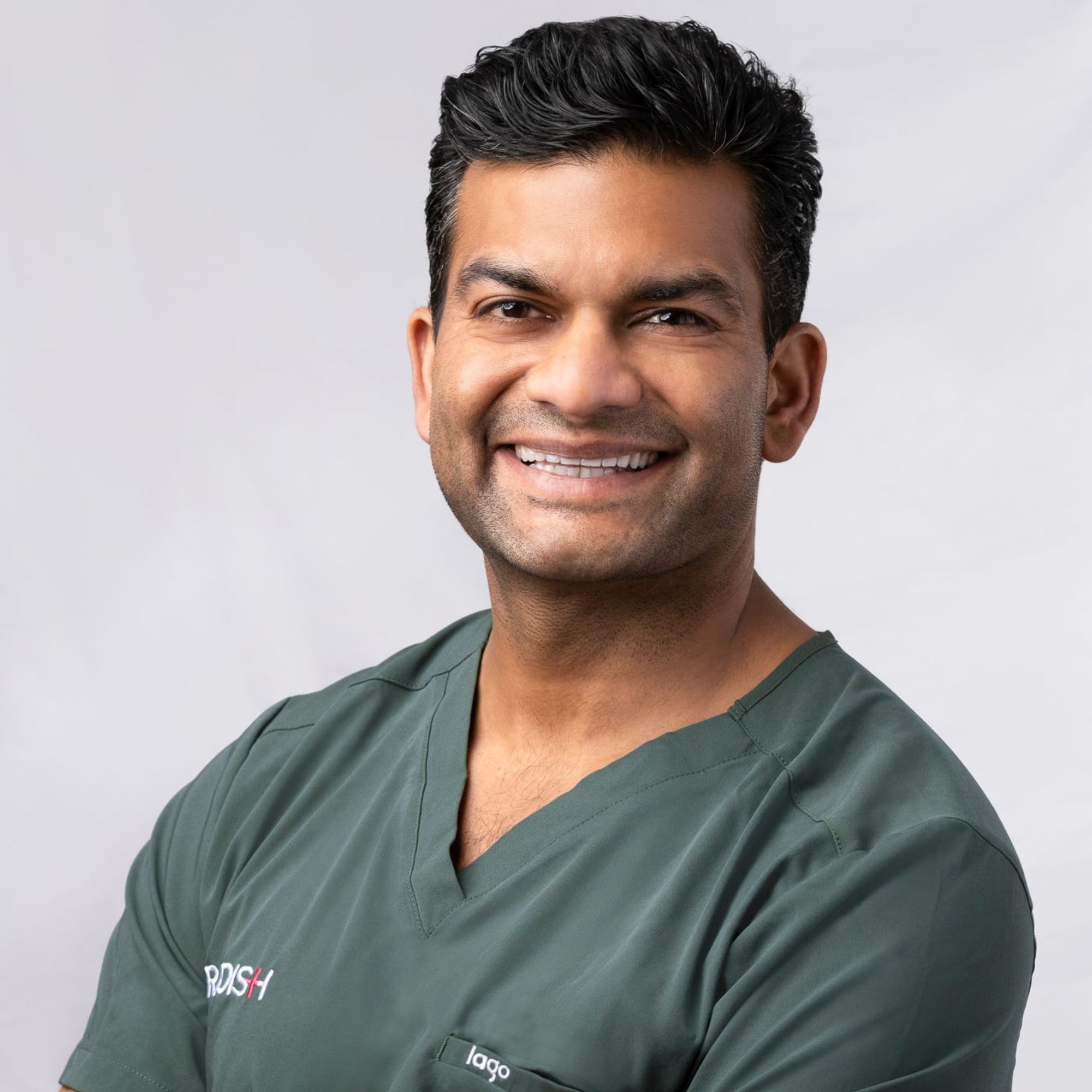
One hundred million Americans have medical debt. It’s a number so large it feels abstract – until you’re the one facing it. This reality drove Veer Gidwaney, fresh off a successful exit from his previous health tech company, to tackle one of healthcare’s most entrenched problems: the declining value of health insurance.
In a recent episode of Category Visionaries, Veer Gidwaney shared how Ansel Health is transforming supplemental insurance through an unexpected platform strategy that’s already attracted Fortune 500 clients. Their approach offers valuable lessons for B2B founders looking to disrupt regulated industries.
The Evolution of Product-Market Fit
“Over the last 15 years, health insurance has continued to get more and more expensive and the value it provides to the end consumer has continued to erode,” Veer explains. This erosion manifests in higher deductibles and out-of-pocket costs, leaving many Americans vulnerable to financial distress from medical events.
But Ansel Health didn’t just see a broken system – they saw incumbent products that had lost product-market fit. As Veer notes, “The incumbent products in this space have not evolved as the market’s needs have changed over the course of the last 15, 20 years.”
This insight led to a critical realization: supplemental insurance wasn’t just underperforming – it was dramatically undersized. “In our view, supplemental insurance as a market should be four or five times bigger than it is today,” Veer shares. The problem wasn’t market saturation, but market activation.
The Platform Play
Instead of competing head-on with established insurers, Ansel made an unconventional choice: they built a platform that powers other insurance companies’ supplemental products. “We have a handful of partners and companies that are well known that have their own versions of our product that they take on the risk. It’s their brand, but it’s running on our platform,” Veer explains.
This strategy solved multiple challenges simultaneously. It gave Ansel instant credibility through established brands, access to existing distribution channels, and the ability to expand the market without fighting incumbents for market share.
But making this work required another crucial decision. “A key decision was to own as much of the platform that runs our product as possible,” Veer reveals. While many startups opt to build on existing solutions, Ansel chose to develop their own technology stack, giving them greater control over automation and partner adaptability.
The Automation Advantage
In insurance, customer experience often determines success. Ansel focused on removing friction through automation, achieving something remarkable: “Three quarters of our claims don’t require the consumer to do anything. We’re proactively paying the claim based upon data that we’re collecting from others.”
This automation-first approach has led to consistently high NPS scores in the 80s – virtually unheard of in insurance. It’s also helped them secure their first Fortune 500 clients and expand to 40 states.
Lessons for B2B Founders
Ansel Health’s journey offers several valuable insights for founders looking to transform regulated industries:
- Value Chain Analysis: Before building, understand how value flows through your industry. As Veer notes, “With insurance, value really comes down to two things: of every dollar of premium, how much goes back to the consumer, and secondly, how often is this product going to get utilized?”
- Market Validation in Regulated Industries: “We were pretty quick about getting the ideas down on paper in a way that we could put it in front of folks who knew a lot about this industry,” Veer shares. In regulated industries, you need both market interest and regulatory feasibility before investing significant resources.
- Platform Strategy: Sometimes the best way to compete isn’t to compete at all. By powering other companies’ products, Ansel gained distribution and credibility while expanding the overall market.
- Technology Ownership: Controlling your core technology can be crucial for automation and adaptability, especially when building a platform others will rely on.
Looking Ahead
Ansel Health’s vision extends beyond just fixing supplemental insurance. As Veer explains, “If everybody can feel secure in the insurance they have related to their health and feel as though that they can deal with any challenges that come their way, then mission accomplished for us.”
With automation driving efficiency, a platform approach enabling scale, and a clear focus on customer value, Ansel Health is demonstrating how thoughtful product strategy can transform even the most established industries. For B2B founders, it’s a masterclass in finding unexpected paths to market leadership.
Actionable
Takeaways
Focus on market expansion through strategic partnerships:
Ansel identified that the supplemental insurance market could be 4-5x larger with the right product. Instead of competing head-on with incumbents, they created a platform that enables established insurance companies to offer their own versions of Ansel's product, leveraging existing distribution channels and brand credibility.
Build for ownership and adaptability:
Gidwaney emphasized the importance of owning their technology platform rather than relying on third-party solutions. This decision enables rapid adaptation to partner needs and efficient automation implementation. They balanced this by building on Salesforce's infrastructure, combining control with scalability.
Validate before building in regulated industries:
When entering regulated markets, Gidwaney's team first validated market interest through conversations with industry experts, then confirmed regulatory feasibility. This two-step validation process ensures resources aren't wasted on technically unfeasible solutions, regardless of market demand.
Prioritize automation for customer experience:
Ansel achieved a high NPS in an industry known for poor customer satisfaction by automating 75% of claims processing. This removes friction from the customer experience and delivers on the promise of "the best insurance product is one you don't have to think about."
Align investors with mission and values:
For products aimed at solving significant social problems, Gidwaney stressed the importance of finding investors who understand and support the mission. This alignment becomes crucial when making decisions that prioritize long-term impact over short-term gains.